Hidden within the vibrant leaves of spinach, the earthy crunch of beets, and the indulgent depth of dark chocolate lies a tiny molecule with a mighty impact: oxalate. This naturally occurring compound, found in a surprising array of healthy foods, has been quietly wreaking havoc on unsuspecting individuals, contributing to a host of chronic health problems. As research continues to uncover the insidious effects of oxalate buildup in the body, it’s time to shed light on this often-overlooked culprit and explore strategies for minimizing its impact.
Oxalates 101: A crash course in chemistry
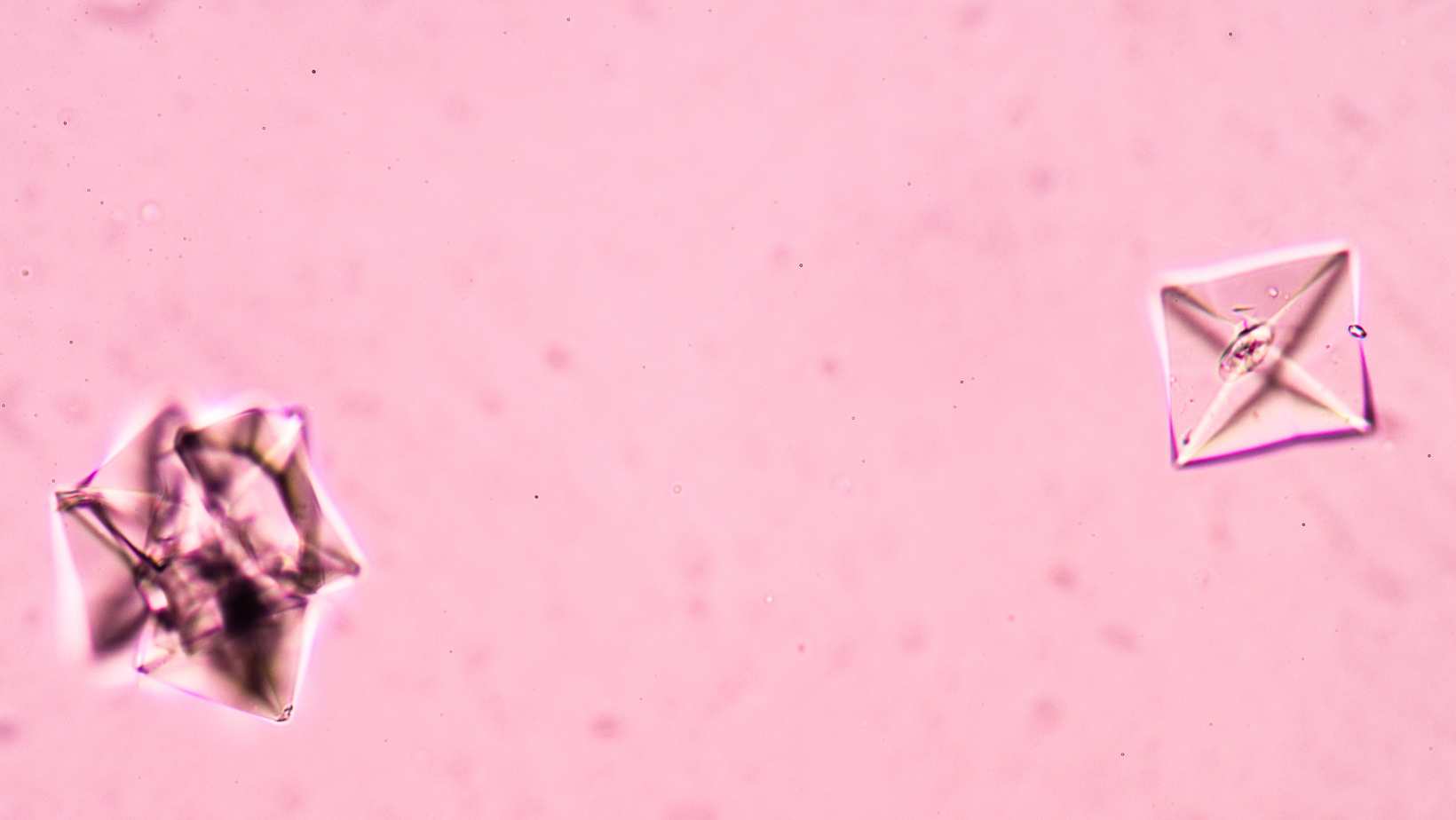
At its core, an oxalate is a simple molecule consisting of two carbon atoms doubly bonded to four oxygen atoms. This unassuming structure belies its powerful ability to bind with minerals like calcium, magnesium, and iron, forming insoluble crystals that can accumulate in various tissues throughout the body. While oxalates play a crucial role in plant defense and mineral management, their presence in the human body can lead to a cascade of health consequences.
The oxalate-kidney stone connection
Perhaps the most well-known manifestation of oxalate toxicity is the formation of kidney stones. In fact, calcium oxalate stones account for a staggering 80% of all kidney stones, affecting millions of people worldwide. As oxalates bind with calcium in the urinary tract, they create sharp, crystalline structures that can cause excruciating pain and damage to the delicate tissues of the kidneys and bladder.
Beyond kidney stones: The systemic impact of oxalates
While kidney stones are the most recognized consequence of oxalate buildup, the effects of this sneaky molecule extend far beyond the urinary tract. As Dr. Sally Norton, a leading expert on oxalate toxicity, explains, “Oxalates can be deposited in virtually any tissue in the body, leading to a wide range of chronic health problems, from digestive issues and joint pain to neurological symptoms and even autism.”
The dietary oxalate dilemma
One of the most surprising aspects of oxalate toxicity is that many of the foods we consider healthy are actually high in oxalates. Spinach, for example, is often touted as a superfood due to its impressive nutrient profile. However, just two cups of spinach can contain up to 1,500 milligrams of oxalates, a significant portion of the daily limit for those sensitive to oxalates. Other seemingly innocuous foods, such as almonds, sweet potatoes, and even tea, can contribute to oxalate overload when consumed in excess.
The metabolic waste factor
While dietary oxalates are a significant contributor to overall oxalate load, it’s important to note that 60-80% of the oxalates in our bodies are actually produced as metabolic waste. This means that even those following a low-oxalate diet may still be at risk for oxalate toxicity if their bodies are not efficiently eliminating this waste product. Factors such as vitamin B6 deficiency, high-dose vitamin C supplementation, and certain fungal infections can all contribute to increased endogenous oxalate production.
The gut-oxalate connection
The health of our gut microbiome plays a crucial role in determining our susceptibility to oxalate toxicity. Certain beneficial bacteria, such as Oxalobacter formigenes, are capable of breaking down oxalates in the gut, preventing their absorption into the bloodstream. However, factors like antibiotic use, inflammatory bowel disease, and gastric bypass surgery can disrupt the delicate balance of gut bacteria, compromising our ability to neutralize oxalates before they can cause harm.
The challenge of oxalate testing
Despite the growing recognition of oxalate toxicity as a contributor to chronic health problems, testing for oxalate levels remains a challenge. While urine and blood tests can provide some insight, they often fail to capture the full extent of oxalate accumulation in the body. As Dr. Norton notes, “Many people with significant oxalate buildup in their tissues may not excrete high levels in their urine, making it difficult to accurately assess their oxalate status.”
The low-oxalate lifestyle: A gradual approach
For those struggling with oxalate-related health issues, adopting a low-oxalate lifestyle can be a game-changer. However, it’s crucial to approach dietary changes gradually to avoid the phenomenon known as “oxalate dumping.” When oxalate intake is dramatically reduced, the body may release stored oxalates from tissues, leading to a temporary worsening of symptoms. By slowly decreasing oxalate consumption and aiming for a daily intake of less than 50 milligrams, individuals can minimize the risk of oxalate dumping and allow their bodies to adapt.
Supporting oxalate detoxification: Key nutrients and strategies
In addition to dietary modifications, several key nutrients and strategies can support the body’s ability to eliminate oxalates and mitigate their toxic effects. Calcium and magnesium citrate, for example, can help bind oxalates in the gut, preventing their absorption. B-complex vitamins, particularly B6, play a crucial role in oxalate metabolism, while sulfur-containing compounds like taurine and N-acetylcysteine can support the body’s natural detoxification pathways.
The power of probiotics: Restoring gut balance
Given the critical role of gut health in oxalate metabolism, incorporating probiotic-rich foods and supplements can be a powerful tool in the fight against oxalate toxicity. Strains like Lactobacillus acidophilus and Bifidobacterium lactis have been shown to degrade oxalates in the gut, reducing their absorption and promoting healthy elimination. By supporting the growth of these beneficial bacteria, individuals can enhance their body’s natural defenses against oxalate buildup.
The oxalate-autism connection: An emerging area of research
One of the most intriguing and controversial areas of oxalate research involves its potential role in the development of autism spectrum disorders. Some studies have suggested that children with autism may have higher levels of oxalates in their bodies, leading to speculation that oxalate toxicity could contribute to the neurological and behavioral symptoms associated with the condition. While more research is needed to fully understand this complex relationship, the possibility of oxalates as a modifiable risk factor for autism has sparked intense interest in the scientific community.
The future of oxalate research: Unanswered questions and promising directions
As awareness of oxalate toxicity grows, so too does the need for further research into this complex and multifaceted issue. Questions remain about the precise mechanisms by which oxalates contribute to chronic disease, the most effective strategies for testing and treatment, and the potential genetic and environmental factors that influence individual susceptibility. By dedicating resources to these critical areas of inquiry, we can begin to unravel the mysteries of oxalate toxicity and develop targeted interventions to protect public health.
Empowering ourselves through knowledge: A call to action
Armed with a deeper understanding of the role oxalates play in chronic disease, we have the power to take control of our health and mitigate the impact of this pervasive toxin. By making informed dietary choices, supporting our body’s natural detoxification processes, and advocating for further research, we can work together to create a future in which oxalate toxicity is no longer a hidden threat, but a recognized and manageable aspect of holistic health. As we continue to explore the intricacies of this fascinating molecule, one thing is clear: the path to optimal wellness begins with knowledge, and the journey ahead is filled with promise and possibility.